Squamous cells are skinny, flat cells that line the surface of the skin, the digestive and respiratory tracts, and certain organs in the body. Squamous cell carcinoma (cancer) can develop in the head and neck area, the skin, cervix, vagina, lung, and anus.
As opposed to a benign tumor, which is non-cancerous, a malignant tumor in the head and neck region refers to a collection of cancer cells growing uncontrollably and may or may not yet have invaded normal healthy tissue. Chemotherapy and other therapies like immunotherapy are used to treat malignant tumors, as they are harmful and potentially fatal.
But, where is head and neck cancer located? Head and neck cancer can be perplexing as it covers a large surface area. So, when someone is diagnosed with this type of cancer, it may need further clarification. Head and neck cancer refers to tumors that develop in one of these many areas: The lip and mouth, the back of the mouth or throat, which is called the oropharynx, the lower part of the throat which is located behind and next to the voice box, called the hypopharynx, the upper part of the throat behind the nose, called the nasopharynx, and the voice box, known as the larynx.
But, what causes head and neck cancer? In the past, the development of head and neck cancer was linked to tobacco and alcohol use. However, in the past 10 years, the development of some head and neck cancers has been linked to infection with certain types of human papillomaviruses (HPV). In fact, scientific data has shown that a type of HPV, called HPV-16 is associated with cancer of the oropharynx and it also causes cervical cancer, as well as anal cancer in men.
While infection with HPV is extremely common, only a small percentage of people can develop cancer from it, primarily because most people's immune systems clear the infection. What's more interesting than discovering the link between HPV and head and neck cancer is the finding that the incidence of head and neck cancers attributed to HPV has increased, while the incidence of head and neck cancers attributed to tobacco and alcohol use has decreased.
According to experts, this could stem from a societal change in sexual activities - specifically, oral sex has become more common. Right now there is particular interest in how to best treat HPV-positive head and neck cancers. Their biology is different from HPV-negative tumors. So, experts are taking a closer look at various immunotherapy strategies to treat HPV-associated cancers.

What are immune system checkpoints?
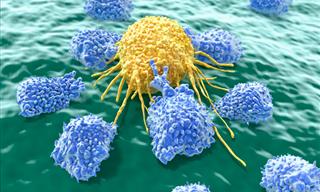
Immune system checkpoints are proteins that are normally located on a person's immune system cells, called T cells. These cells are like policemen that seek out trouble, which in this case would be cancer or infection, within the body. When these T cells encounter another cell, it evaluates the cells using proteins located on its surface to determine if the cell is 'normal' or 'abnormal'. If abnormal, the T cell will initiate an attack against the cell. So, you may be wondering, during this attack, how are healthy cells protected. This is where checkpoint proteins come into play. Checkpoint proteins lay on the surface of T cells and end ensure that healthy cells are left alone.
But cancer is devious. It actually makes these checkpoint proteins (a true copycat) to avoid an attack from a person's immune system. A checkpoint protein is expressed on the surface of cancer cells to sneak by the immune system is known as PD-1.
Now scientists have discovered that they can block PD-1 on cancer cells so that cancer is detected by a person's immune system. This is where immunotherapy comes into play, and these PD-1 blocking drugs are called immune system checkpoint inhibitors.
But, how can immunotherapy treatment help? There are two immune system checkpoint inhibitors that were FDA approved in 2016 for treating people with metastatic and/or recurrent head and neck squamous cell carcinoma. Metastatic cancer refers to head and neck cancer that has spread to other areas of the body. Meanwhile, recurrent head and neck cancer refers to cancer that has progressed despite treatment with a platinum-based chemotherapy regimen. These two immunotherapies are called Keytruda (pembrolizumab) and Opdivo (nivolumab).

Pembrolizumab
Early studies show that pembrolizumab has a good safety profile and can be effective in shrinking some people's cancer. In one phase II study, 171 people with head and neck cancer which had progressed, although patients had been treated with chemotherapy, had received an infusion of pembrolizumab every three weeks. The response rate was 16%, and the median duration of response was 8 months. The response rate refers to the percentage of participants whose cancer shrinks or disappears in response to the treatment. With regards to safety, it was found that 64% of participants had experienced a treatment-related adverse effect, but only about 15% had experienced a grade three or four adverse events - perceived to be severe or life-threatening.
The most common side effects noted were fatigue, hypothyroidism (underactive thyroid gland), nausea, elevation of a liver enzyme and diarrhea. Still, receiving immunotherapy is a delicate process as the body and the medication work together to determine what is bad (cancerous) and what is normal and healthy. Phase II studies are currently ongoing. At this stage, it will be compared against the standard of care medication to see how it fares, and whether it is more effective.
Nivolumab
In a phase III study, over 350 people with recurrent/metastatic squamous cell carcinoma of the head and neck, whose disease had progressed within six months of receiving platinum-based chemotherapy, were randomized to receive either nivolumab every two weeks. The nivolumab is given as an infusion through the vein, or as a standard therapy, methotrexate, docetaxel, or cetuximab. Results showed a significantly longer overall survival in the people who received nivolumab versus those who received the standard therapy. In addition, the one-year survival rate was 36% in the bivolumab group, in comparison to the 16.6% in the standard therapy group. In other words, the one-year survival rate more than doubled.
Adverse effects occurred in 13% of the nivolumab group versus 35% of the standard therapy group. In the nivolumab group, the most common effects were fatigue, nausea, rash, decreased apetite, itching and general effects related to the thyroid, where 7.6% developed hypothyroidism.
Without a doubt, it appears that immunotherapy is changing the face of cancer treatment. Still treating head and neck cancer is a complex process and the best you can to is remain an advocate for your cancer health by gaining knowlege.
 Go to BabaMail
Go to BabaMail